In the first Sweep the Sun columns we looked at the Gold Standard ISO 24444:20191 and the possible alternatives that are currently in the making at ISO2. This time we look at “outdoor SPF testing” which had its origins in Schulze’s first definition of SPF3 and has now being revisited by some who want to measure sun protection performance under more realistic conditions4. It has long been known that the minimal erythema dose (MED), i.e. the endpoint in the SPF determination is not the same when irradiated with a laboratory lamp as it is outdoors in the sun 5, 6. However, only recently has there been growing interest in this difference. Reasons for this may be the higher SPF values now available and the greater variability associated with them, which has led to more skepticism about the efficacy of sunscreens. A few years ago, I asked Brian Diffey to investigate this difference between SPF measurement in the laboratory and outdoors from a theoretical perspective. We concluded that products labeled SPF50+ may not provide more protection against the full spectrum of sunlight than those with SPF257. The original SPF determinations were performed outdoors with natural sunlight. For practical reasons, the natural light source was replaced by a standardized lamp (Figure 1). However, the awareness that the radiation spectrum of the lamp differs significantly from natural sunlight was lost. The SPF determined with artificial sunlight according to ISO24444 (as indicated on all sunscreens currently on the market) is too high due to the lack of the entire radiation spectrum7, 8.

Based on experimental work, two research groups had already pointed out this phenomenon. However, their publications received little attention5, 6. Hughes and others support this earlier work and the assumption of Diffey and Osterwalder with more recent in vivo studies in humans with natural sunlight4, 9. In fact, it was this more recent experimental work of Shaun Hughes that triggered and inspired our theoretical work7. But only recently have Hughes et al published some of their extensive experimental work (Figure 2). The surrogate for sun protection performance was the percentage of skin sites that exhibited erythema. According to the old notion of the SPF as multiplier of self-defense time, none of the subjects treated with high SPF sunscreens should have shown any signs of erythema after (only) 2 hours of exposure time.
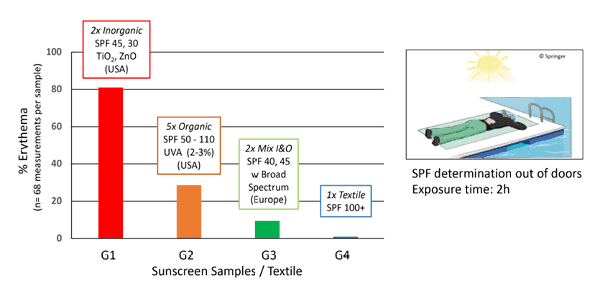
Approximately 80% of the skin areas were erythematous with 2 products (G1, USA), nearly 30% with 5 products (G2, USA), and approximately 10% with 2 products (G3, Europe). The fabric of the protective clothing (G4), under which no erythema could develop, served as a quasi-negative control for each subject. The two sunscreens with SPFFDA 30, 45 (G1, USA) showed significantly lower protection compared to the sunscreens with SPFFDA 50-110 (G2, USA). The two sunscreens with SPFISO24444 40, 45 (G3), which contained broad spectrum UV filters, clearly showed the best protection compared to the product groups (G1, G2). The experiment clearly shows that not only the SPF value is decisive for comprehensive protection, but also the broad protective effect of a product due to the presence of broad-spectrum UV filters (G3). The best protection is achieved through clothing (G4), which reduces the entire spectrum of light evenly (according to the Anglo-Saxon protection slogan ‘‘cover up’’). This ideal situation has coined the term spectral homeostasis10.
The question arises as to why we see so much erythema with these relatively high SPF sunscreens after only 2 hours of exposure. Here are some possible reasons.
– Visible light has an effect on the minimum erythema dose, as outlined in (7).
– Some sunscreens may be mislabeled (SPF values not as high as indicated).
– SPF measurement outdoors may have some errors.
From these experiments alone, we cannot give a definitive answer. However, we can conclude that the type of sunscreen plays a role, i.e., European sunscreens perform better because they cover a broader UV spectrum. And textiles perform better because they cover not only the entire UV range, but also visible light.
The examples of the outdoor tests by Hughes et al. show that there are differences between sunscreens and between sunscreens and textiles. In short, the sunscreen closest to the textile is the best/ideal sunscreen, also known as spectral homeostasis protection. This means that sun protection performance is not reflected in SPF alone, but that the broad-spectrum aspect plays an important role in protecting against erythema, skin aging and skin cancer.
In summary, the answer to the question of whether we should or will return to outdoor SPF testing is a resounding NO. As a routine method, it would simply be too complicated. That said, we must remember and be aware that neither the current SPF gold standard, ISO 24444:2019, nor any of the upcoming alternative methods, such as ISO/CD 23675 or ISO/CD 23698, accurately reflect reality. No standard does. Therefore, interpretation of the results of such standards is critical. In the past, SPF values were over-interpreted as a multiplier to determine how long a person could stay in the sun. Today we know that it should not be used in this way. SPF is a relative measure of sunscreen, and we must remember that it is not only SPF that matters, but also UVA protection, especially when it comes to skin cancer prevention. The UVA-PF should be at least 1/3 of the SPF according to the European recommendation of 2006. Making the UVA-PF higher than 1/3 of the SPF is possible, but also a real challenge for the formulator.
We will talk more about this in the future.
References:
1 ISO 24444:2019 Cosmetics – Sun protection test methods – In vivo determination of the sun protection factor (SPF), https://www.iso.org/standard/72250. html, Viewed 5.5.22
2 Cosmetics Europe Recommendation No. 26 on the use of alternative methods to ISO 24444:2019, 2022-03-23, Cosmetics Europe Recommendation No. 26 on the use of alternative methods to ISO 24444:2019, 2022-03-23, Viewed 5.5.22.
3 Schulze, R., Einige Versuche und Bemerkungen zum Problem der handelsüblichen Lichtschutzmittel. Parfümerie und Kosmetik, 37 (1956) 310-315.
4 Granger, C., Krutmann, J., Bustos, J., Sola, Y., Hosenally, M., Trullàs, C., Andres, P., and Passeron, T., New Methodology to Evaluate Sunscreens Under Outdoor Conditions: A Double-Blind, Randomized Intra-Individual Clinical Study of a Water-Based Broad-Spectrum SPF50+ Versus SPF15 (P3) and SPF50, Dermatol Ther (Heidelb), 9 (2019) 589-599.
5 Brandt, M., Rohr, M., and Schrader, A., Influence of VIS/NIR Radiation on the Characterization of Sunscreens and Human Skin, IFSCC Magazine, 4 (2001) 15-19.
6 Lott, D., Testing SPF 15-100, Indoor vs. Outdoor, Cosmetics&Toiletries, 128 (2013) 638-647.
7 Diffey, B., and Osterwalder, U., Labelled sunscreen SPFs may overestimate protection in natural sunlight, Photochem Photobiol Sci, 16 (2017) 1519-1523
8 Diffey, B., Natural and Simulated Solar Radiation, Curr Probl Dermatol, 55 (2021) 44-52.
9 Hughes, S.N.G., Lowe, N.J., Gross, K., Mark, L., Goffe, B., Hughes, H., and Cole, C., Assessment of Natural Sunlight Protection Provided by 10 High-SPF Broad-Spectrum Sunscreens and Sun-Protective Fabrics, Curr Probl Dermatol, 55 (2021) 157-169.
10 Dudley, D.K., Laughlin, S.A., and Osterwalder, U., Spectral Homeostasis – The Fundamental Requirement for an Ideal Sunscreen, Curr Probl Dermatol, 55 (2021) 72-92



